Rekapitulation
- 15 Aufrufe
By Allan A. Abbass | Joel M. Town
Abstract: Intensive short‐term dynamic psychotherapy (ISTDP) was developed to manage treatment impasses preventing the experiencing of feelings related to childhood attach- ment interruptions, such as parental loss. According to ISTDP theory, certain categories of patients will exhibit habitual patterns of responding within the treatment relationship (called defenses) to certain anxiety‐ provoking thoughts and feelings. Such defensive beha- viors interrupt awareness of one's own feelings, self‐ directed compassion and engagement in close human attachments, including the bond with the therapist. Rupture‐repair sequences in ISTDP are primarily con- sidered in the context of a patient's defenses and the responses a therapist has to these defenses. By under- standing and clarifying these defenses, this risk of sub- sequent misalliance, that is negative shifts or ruptures in the alliance, are minimized. In this paper we summarize ISTDP theory and technique through the use of clinical vignettes to illustrate defense management as a rupture‐ repair equivalent in ISTDP.
Faculty of Medicine, Centre for Emotions and Health, Dalhousie University, Halifax,
Nova Scotia, Canada
KEYWORDS
emotion, intensive short‐term dynamic psychotherapy, psychodynamic, rupture‐repair processes, unconscious, unconscious therapeutic alliance
1 | INTRODUCTION
Ruptures in the therapeutic alliance, which if not repaired, may lead to negative treatment outcomes including drop‐out from therapy (Eubanks et al., 2018). Ruptures have been defined as observable behaviors, or “markers,” in which a patient begins to “confront” or “withdraw” from their therapist (Eubanks et al., 2015). Such a break in the alliance may reflect a disagreement between patient and therapist regarding the goals and/or tasks of therapy, which puts a strain on their emotional bond (Safran & Muran, 2000). In this article, we present the perspective that in order for meaningful change to occur for some patients, it may be both expectable and, in fact, necessary for such rupture markers to manifest with the therapist in‐sessions. We suggest that through the development of patient insight and mobilization of their motivation to make changes, as well as creating a climate for encouraging the experiencing and expression of emotions, what could be conceptualized as a process to be avoided, may in fact be a positive process to be welcomed.
Frustrated with the mixed effects of long‐term psychoanalytic psychotherapy and limited resources in the public mental health system, Dr. Habib Davanloo began to develop his model of intensive short‐term psychody- namic psychotherapy (ISTDP) in Montreal in the 1970s. Using video technology, he studied the treatment ingredients that appeared to accelerate access to feelings related to trauma that ordinarily triggered a patient's anxiety and avoidance, and subsequently produced current character and symptom disturbances. Based upon this study, he developed a model of brief psychodynamic therapy that emphasizes the central impact of interrupted childhood attachments in contributing to a broad spectrum of symptom disorders and personality disorders (Davanloo, 1990). Drawing on Bowlby and other theorists, Davanloo highlighted the centrality of attachment experiences with caregivers in human development (Bowlby & Gatling, 1988). Interruption of positive attachments is what Davanloo referred to as attachment trauma. Such attachment interruptions in childhood result in a series of mixed feelings, that when not worked through, can be reactivated in later relationships resulting in problematic patterns of symptoms and interpersonal difficulties; in the caring setting of a treatment relationship, these acti- vated feelings and defenses can contribute to treatment misalliance and negative outcomes. For example, a 3‐year‐ old child whose father suddenly dies may have intense grief about this attachment loss. The intense pain of the grief and relative absence of other attachment figures to help tolerate and understand these feelings, may leave the child to learn to ignore and avoid these feelings. These feelings stay unresolved and cause anxiety and avoidance of relational experiences that involve closeness, thus, undermining the development of healthy attachment with others.
Davanloo described two spectra of patients who have experienced various degrees of attachment trauma that have not been worked through. These two spectra describe the effects of trauma through the development of habitual, often implicit, patterns (referred to as defenses) a person can be observed to exhibit in response to feelings being activated in a relational context. He noted that anxiety signals the emergence of feelings that need to be defended against or avoided using various defense mechanisms. Based upon the degree of unresolved attachment trauma experienced, patients experience more or less disabling patterns of anxiety (severity determined by the negative impact on bodily muscles, organs or cognitive functioning) and defenses that, for example, aim to evade, distance, control or provoke other people. The term resistance is used to describe defenses when they are actively being used in treatment. Thus, defenses are habitual responses aimed to prevent the emergence of feelings by preventing having a collaborative, trusting relationship with the therapist.
The first spectrum Davanloo described, reflects an increasing degree of resistance, from low resistance to manifestations of high resistance. Patients on this spectrum have in common the ability to maintain a level of reality testing, even when highly anxious and avoidant of uncomfortable feelings or relational experiences, allowing them to at least partially recognize their feelings are impacting their perceptions of themselves and others. Low resistance manifests as patients who have unprocessed grief about losses that occurred later in childhood and afterward; such patients typically have a range of adaptive means of coping alongside only minor defenses, such as the use of vague language, and mild symptoms such as mild muscle tension. For example a girl whose father died when she was a teen became nervous and tended to emotionally detach when she had her first boyfriend some years later; the grief about her father's death was activated by this new attachment resulting in muscle tension and a tendency to avoid closeness (Abbass, 2015).
Moving across the spectrum, moderate resistance is operationalized as individuals who have often had some positive early life relationships alongside attachment trauma in middle childhood and have symptoms and character patterns which are disturbing to them; they are often partially aware of their defensive coping patterns and they try not to use them in a service of maintaining a relationship with the therapist. For example, moderately resistant patients are aware that they become tense, ruminate, and distance themselves when there is a moment of closeness: though they are aware of it, they do it anyway and thereby prevent themselves from closeness and from being aware of the feelings they avoid.
On the other extreme of this first spectrum is high resistance that manifests as entrenched maladaptive character patterns and defenses with which the patient is strongly identified. For example, the person may tend to be defiant and controlling of others, while being unaware how these patterns contribute to involuntarily keeping the therapist at a distance. Highly resistant individuals have typically endured extensive and often repeated attachment ruptures in childhood, leading to formation of automatic and pervasive patterns of thinking and be- having that prevent closeness and the emergence of feelings related to past attachment ruptures. Intense early attachment trauma cause high levels of unresolved grief, rage and guilt about rage that are understood to fuel a self‐defeating tendency that manifests as a firm belief that they are not deserving of positive experiences and should accept negative treatment from others. In the setting of a caring therapist, these patients become tense and automatically behave in ways to control (such as by defiance), devalue (such as by being critical), self‐criticize or detach from the therapist (such as by going silent and withholding all eye contact).
Some highly resistant patients have more limited anxiety tolerance and have difficulty self‐reflecting on emotional processes (Abbass, 2015; Davanloo, 2001). Anxiety manifests as stomach upsets, diarrhea, migraine headaches, blood pressure changes and muscle weakness. They commonly experience major depression and fatigue. This group of patients do not use the distancing defenses described above and rather tend to become fatigued and physically sick in treatment sessions. Treatment in this group involves first improving the ability to identify anxiety and underlying feelings to build anxiety tolerance (Abbass, 2015).
The second spectrum Davanloo described is the spectrum of patients with fragile character structure. Com- pared to the aforementioned spectrum, this spectrum is characterized by more severe personality problems and greater difficulties containing intense feelings, such as grief, rage, and guilt from early and severe attachment interruptions such as repeated neglect in infancy resulting in disorganized attachment (Granqvist et al., 2017). These intense feelings cause acute spikes in anxiety in relational experiences that disrupt cognitive‐perceptual function, such as the ability to think (e.g., cognitive confusion) and to perceive via sensory experiences (e.g., blurred vision, impaired hearing). In these cases, a defensive process enables the mind to split off and project out feelings such that they can be disowned. For example, when these patients feel angry at the therapist, they may begin to believe the therapist feels angry at them. They experience a broad range of symptoms and typically meet criteria for dissociative disorder along with various types of personality disorders including borderline personality disorder (Abbass, 2015; Davanloo, 2001).
The presumed central mechanism of change in ISTDP is enabling the patient to begin to safely experience the feelings related to past and current attachment relationships that have previously caused a flood of anxiety and defenses. Compared to traditional analytic therapy, in ISTDP, the therapist assumes a more active role through exploring and establishing key areas of focus by asking about and highlighting situations in which feelings, anxiety and defenses emerge. Through positioning the therapist's chair so they are sitting face‐to‐face with the patient and asking about the here‐and‐now of the therapeutic relationship, the therapist explicitly communicates an intention to be engaged. The culture of requesting sessions be video‐recorded as part of the treatment process may equally contribute to this therapeutic climate and the ‘intensive' nature of the approach. The method varies to titrate the anxiety provoking emotions that will be triggered, thus aiming to tailor the moment‐to‐moment response according to the capacities and category of patient. For example, cases with low resistance will quickly move to talking about the loss of a loved one that precipitated their difficulties: focus on the loss and encouraging the patient to be present with the memories of closeness with the loved one is enough to facilitate the experience and working through of grief to bring symptom resolution.
FIGURE 1 Process of intensive short‐term dynamic psychotherapy in the highly resistant patient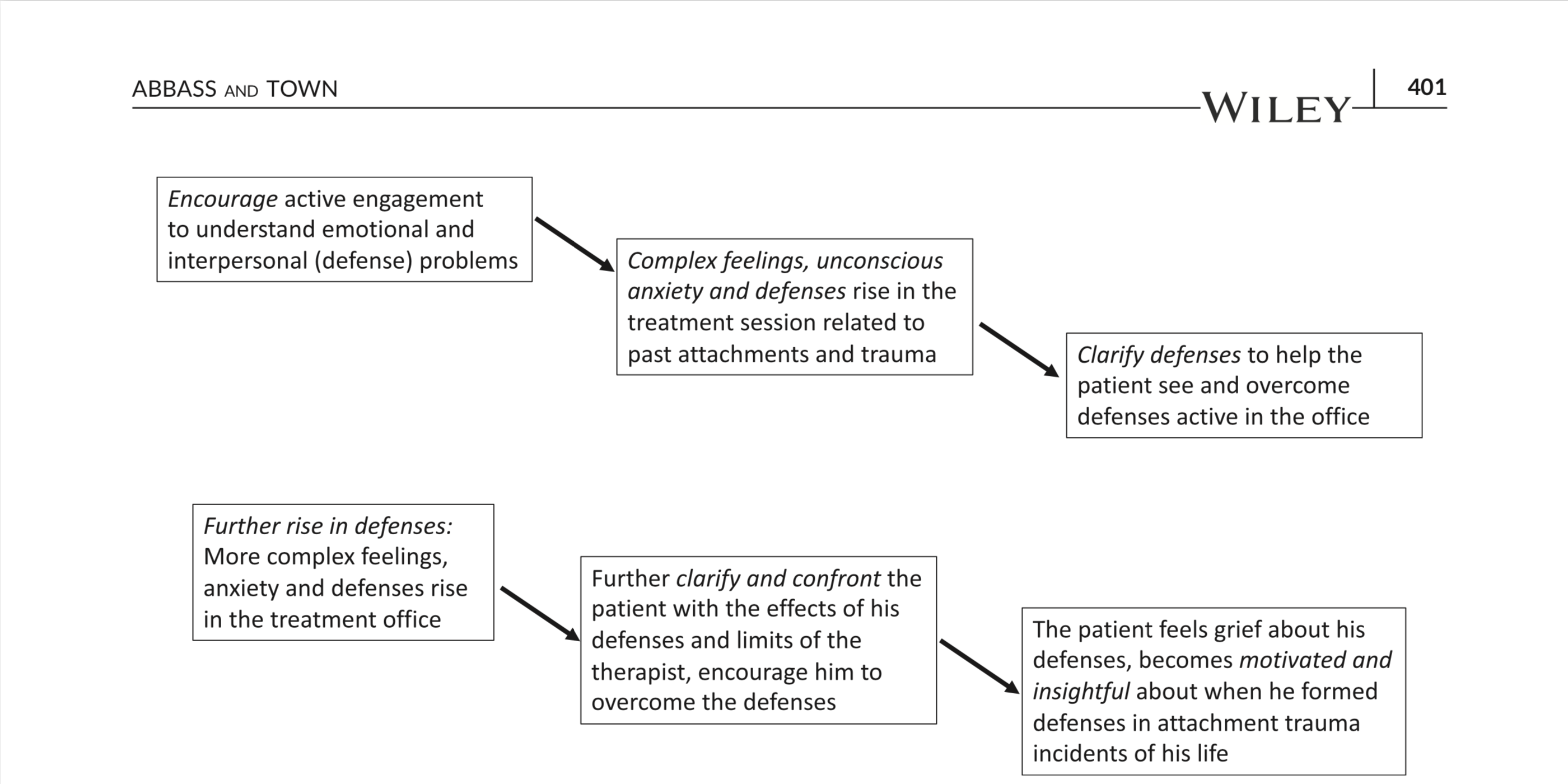
The process with cases of high resistance, on the other hand, is more complex (Figure 1). Through a series of specific, tailored interventions, the therapist cultivates a clear focus on how a patient's habitual responses to anxiety provoking feelings—defences creating resistance in the office—relate to their presenting difficulties and potentially defeat the treatment itself. This is designed to identify and handle alliance threats as they arise. First, pressure or interventions recognized as encouragement and focus from the therapist, are used to establish healthy self‐examination about problems areas and relational patterns toward building openness and collaboration with the therapist. This involves asking specific and direct questions about topics that appear to be related to the person's difficulties, then asking the patient to talk about their feelings towards others during those situations. This effort mobilizes mixed feelings including appreciation and irritation with the therapist that are mirror images of mixed feelings the patient felt during traumatic attachment experiences; Davanloo refers to these as complex transfer- ence feelings to indicate that old feelings are transferred onto the therapist (herein we will refer to these as complex feelings). For example, a woman who was extremely scared of her violent father but also craved a close relationship with him, may initially be afraid of her therapist while at the same time seeking the therapist's approval and attention: such mixed feelings may manifest as muscle tension and a tendency to avoid eye contact with the therapist.
As these feelings rise, unconscious anxiety is activated, and can be observed through muscle tension in the patient's body with hand clenching and sighing. It is referred to as unconscious anxiety because typically a person is at first unaware that their body is displaying markers of anxiety or what they are anxious about. For example, a patient who can cognitively identify frustration related to being “dismissed by their boss,” may at first clench his hands and sigh then start to rationalize away his feelings by saying “my boss is under a lot of pressure.” This anxiety in turn activates unconscious defenses in the presence of the therapist that in summation are resistance in the form of a wall of mechanisms preventing openness, collaboration and healthy self‐examination. These defenses interrupt the patient's own treatment goals (e.g., treating chronic anxiety), hence, they become self‐defeating and relationship‐defeating in their current function. If these defenses are not recognized and managed, the therapist may become entangled in them, leading to poor treatment alliance and treatment impasse. For instance, with a patient who habitually rationalizes away their anxiety provoking feelings, therapy could easily become an intellectualized conversation leading to therapist and patient feeling demoralized and ineffectual. To help the patient recognize and understand these defenses, first the therapist clarifies the defensive behaviors and the impacts they have: he may say for example “do you notice that you avoid my eyes when you talk about how you feel with your wife?” Then to enable the patient to stop using the defenses, the therapist and patient confront or challenge the defenses to interrupt and undermine the avoidant behaviors:
for example, the therapist may say, “so if you don't become detached, let's see what feelings are coming up.”
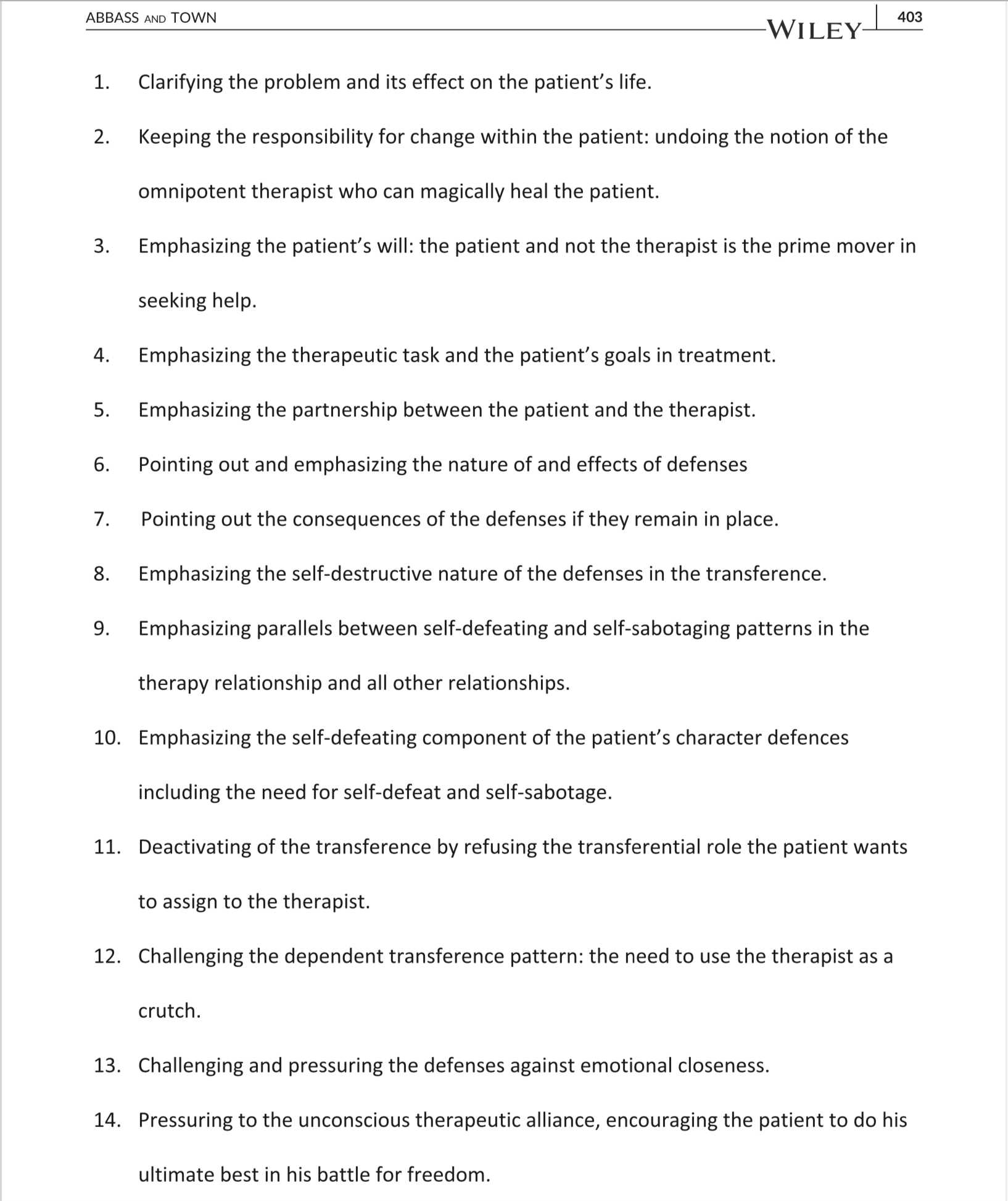
If defenses mount further in the session, then more elaborated and lengthier clarifications and challenges to the defenses are used, comprising what Davanloo called head‐on collision (Davanloo, 2000). Head‐on collision involves spelling out for the patient the impact of these defensive behaviours on their treatment. For example, the therapist may state “as long as you stay detached and distant here with me, I will not be able to know you and you are left in there on your own to battle these problems”: instead of becoming annoyed that the patient is detaching, the therapist points out the self‐defeating pattern and encourages the patient to overcome it. Through such a focus, what could otherwise be another misalliance, whereby the patient persistently avoids talking about feelings in the safety of treatment and gradually disengages, is turned into a therapeutic victory for the patient over his own destructive tendencies. Some of the tasks of head‐on collision are described in Figure 2. Through these therapist efforts, the patients turn against their defenses and feels sadness about the consequences of these self‐defeating behaviors: they have a deep realization that they are interrupting the close and open moments with others they most desire.
Throughout this process, the therapist aims to extract themselves from any interaction where they could be seen as omnipotent or trying to control the patient: such a situation could create a power struggle so must be avoided, if possible, or handled as it emerges. For example, to avoid getting in an omnipotent position, the therapist invites his patients to make their own decisions about each step of the process. For example, they may say, “if you wish, we can examine why you ignore your own feelings like this, but only if it is your wish to do so.” Such clarity about patients making their own decisions prevents a situation where patients defy the therapist or passively comply with the therapist.
A unique feature of this treatment sequence is the view that resistance can be more directly addressed and confronted to improve and protect the therapeutic alliance. This is analogous to helping the patient to “take down” a metaphorical wall of defenses, rather than “stepping back in frustration and attempting to walk around an endless wall.” With the gradual weakening of the resistance and a growing understanding of the defensive process, the patient becomes more open with the therapist. This in turn activates more feelings about past interrupted relationships as well as more anxiety and corresponding self‐protective behavior. Again, the therapist helps the patient see and turn against these defenses in sequence as they arise. The therapist may say
“again you become detached and put the wall back up here with me, but if you keep this wall it will defeat what you are trying to do here with me.” This study brings a greater rise in feelings linked to past attachment experiences and trauma.
Such close contact and focus on ways the patient inadvertently avoids closeness, stirs more and more unresolved complex feelings about previous disrupted attachments. As these complex feelings are mobilized, a dynamic force Davanloo called the unconscious therapeutic alliance (UTA) is activated (herein operationalized as the emergence of patient insight and motivation). This clinical phenomenon is likely common in positive treatment processes regardless of model. It may parallel “aha moments” or the spontaneous awareness of the past origins of behavioral patterns seen in diverse therapy models. The emergence of patient insight and motivation is conceptualized as a force linked to drives for attachment and healing: as it activates, it brings self‐understanding, linkages and images, such as a vivid memory of an event related to past attachment trauma. For example, the patient may spontaneously see, hear and even smell the living room where her brother was being battered by her father. At these times, the process is relatively smooth, without anxiety and defenses working, and the patients can make their own insights and linkages between past and present experiences. This phenomenon of increased patient insight and motivation comes in direct proportion to the complex feelings and the experience of these feelings with the therapist, coupled with work against the defenses, are considered key to accessing the feelings about at- tachment trauma (Abbass & Town, 2013).
FIGURE 2 Tasks of the head on collision (After Abbass, 2015)
For patients who have poor anxiety tolerance or a fragile character structure, the treatment process focuses on first building capacity for anxiety regulation before underlying feelings can be safely accessed. Fragile patients typically require more time and support in‐sessions to establish a conscious therapeutic alliance for this task than patients who do not have the same manifestations of fragility (as previously described). This process is much more of a supportive process, devoid of challenge and head‐on collision, thus, it is modified to address the unique limitations of these patients. With all patients, conscious therapeutic alliance is formed by shared goals, coregulation of affect, co‐summarizing of the findings from the session and other actions that are common factors of psychotherapy. In contrast to working with resistant patients, indicators of the patient confronting or withdrawing from the therapist (ruptures) aim to be avoided with fragile patients through continually co‐monitoring the shared process and progress. With fragile character structure patients, the alliance is vulnerable to collapse because the therapeutic process is consistently creating more anxiety than the patient is able to regulate. At these times, based on ISTDP principles, the fragile patient is automatically likely to cope though implicitly disowning strong negative feelings triggered about the past; for instance, they cannot tolerate seeing themselves as feeling angry, as this would implicitly parallel feelings about past trauma, so instead, they project that the therapist is angry at them.
Rupture markers described by Eubanks et al. (2018), such as patient withdrawal or confrontation with the therapist, may be characterized in ISTDP terms as related to a build‐up of patient defenses in the therapeutic relationship. Empirical evidence for this includes the classification of an anxiety‐based state of “fear” being present (Kramer et al., 2014) and more frequently observed defenses (Gerostathos et al., 2014; Michel et al., 2011) in rupture sessions. In contrast, the resolution phase is characterized in ISTDP terms as potentially greater agreement on task and a stronger patient‐therapist bond, alongside greater patient insight and motivation relative to the observed presence in‐sessions of unconscious defenses and anxiety. Evidence for this comes from Kramer et al.'s (2014) finding that in the post‐rupture sessions when resolution occurs, patients exhibited higher levels of affect, specifically expressing and experiencing grief and anger about autobiographical life events. There is limited psy- chotherapy research studying the session‐to‐session associations between alliance development and patients ex- periencing and expressing previously avoided feelings. A preliminary finding from a small case‐series design to study session‐to‐session processes in ISTDP, showed that increased in‐session patient affect experience, manifest as increased motivation and insight, predicted a stronger alliance in subsequent sessions (Town et al., 2013). This contrasts the common finding that the conscious alliance is a foundation for change as it is in all forms of psychotherapy.
ISTDP theory and technical recommendations describe combinations of specific therapist responses, based upon patient responses, to guide the treatment process. For example, treatments that primarily use encouragement to identify a patient's underlying feelings (e.g., Abbass, et al., 2009) are more likely to be associated with higher levels of immediate patient affect experiencing (Town et al., 2012, 2017). Indeed, studies across different psychodynamic treatment models suggest that the specific nature of therapist in- terventions are associated with alliance patterns and development during therapy. For instance, Gerostathos et al. (2014) found that in resolution sessions, compared to control and rupture sessions, therapists exhibited higher rates of interventions that addressed patient defenses. Early research showed that the accuracy of clarifications and interpretations predicted the development of the alliance (Crits‐Christoph et al., 2003) and treatment outcome (Crits‐Christoph et al., 1988). Building upon this, Sahli et al. (2015) found that accuracy of therapist interpretative interventions in rupture resolution sessions related to outcome. In addition to process research, ISTDP has been evaluated through over 50 studies and shown effective (Abbass et al, 2012) and cost effective (Abbass & Katzman, 2013), including in the treatment of complex and refractory patient populations (Abbass, 2016; Abbass et al., 2015).
2 | CASE PRESENTATION: THE CAVEMAN
2.1 | Presenting problems and patient description
This previously published case material has been revised and adapted to formulate the case from the rupture‐repair model. At the time of treatment, this patient was a university educated, caucasian, 57‐year‐old man with a history of dysthymic disorder, major emotional detachment, distancing, and defensiveness that prevented him from ever establishing close relationships. He was also chronically self‐defeating, self‐critical and felt he deserved bad things. He was formulated as a highly resistant patient from the spectrum of resistance described above. He had a past history of alcoholism and drug addiction. Diagnostically, he met criteria for narcissistic and avoidant personality disorders. Over the previous 30 years he had seen a large number of therapists. Some of these therapy efforts lasted only minutes and ended with him leaving the office with no hope the therapist could help him. He had the irresistible tendency to undermine therapists, to devalue and outsmart them. Within the setting of a hospital based, outpatient psychotherapy services, he was referred by his treating therapist (a male psychiatrist with 7 years of training and experience in ISTDP) to a male psychiatry colleague and supervisor (with approximately 20 years of experience with ISTDP). This followed about 25 ISTDP sessions, at which point a single trial therapy consultation was suggested to help address poor treatment alliance with his therapist: the therapist and patient became entrenched in theoretical arguments in the treatment sessions, preventing access to underlying anxiety‐provoking feelings that were impairing his life. The treatment had reached a stalemate and both the patient and therapist were coming to believe the treatment should be terminated (Abbass et al., 2015).
2.2 | Case formulation
Based on previous treatment sessions with his therapist and information we will see in this interview, this patient had been hurt greatly in close relationships by both of his parents: his father had been violent and verbally abusive while his mother was affectionate but passive and ineffective in protecting the children. These attachment inter- ruptions produced a cascade of complex feelings including sadness, rage and guilt about rage. Because of anxiety about these intense feelings, he developed a pattern of avoiding others, controlling others and criticizing others in his limited relationships and also with the therapist. He tended to be extremely competitive and wanted to “defeat”others and this would be enacted when the therapist attempted to establish common goals in therapy. In addition to this, he was also self‐defeating and self‐punitive believing he did not deserve to enjoy life, thus discussions about motivation for change with his therapist were quickly dismissed. Hence, interpersonal relationships (including in therapy) generated unconscious anxiety and unconscious defenses, as described above, to keep away emerging feelings of grief, rage, and guilt and to prevent closeness, with the risk of being hurt again.
2.3 | Course of the trial therapy session
The first minutes of this interview involved motivating the patient to examine his problems of emotional detachment, distancing, and self‐defeating behavior patterns, with the aim of helping him to recognize and to dislike his use of these defenses. Focusing on his defenses of detachment, distancing others and self‐deprecation and their impact in his life, stirred painful feelings of grief about hurting himself and others through his inadvertent use of these habitual behaviors. Following is a segment 10 min into the interview.
Th: So, the thing is that when you're coming here you've been working to undo this notion that you deserve negatives, that you deserve some bad things. To override that. (Focus on the task to overcome his self‐defeating tendency).
Pt: Yeah.
Th: To replace it with that you deserve the good things. That's what you're working on? (Clarification of the task of that moment, focus on self‐compassion).
Pt: But apparently, I'm too smart for my own good.
Th: So, is there some reason for that? Are there some crimes you did that you feel you deserve a bad thing? (Rhetorical question to the healthy side of the patient).
Pt: Yeah.
Th: Who did you hurt?
Pt: Lots of people. I hurt people by not returning their affection. I mean I didn't love my mother enough. I wanted my father's affection too much.
Th: You mean you kept them away; you mean you kept your parents at a distance?
Pt: Probably my mother. I didn't tell her enough that I loved her.
Th: So, you didn't give her enough love?
Pt: Yeah.
Th: So, you didn't give her all the affection you wanted to give her—you withheld.
Pt: Yes.
Th: So, what happened eventually with your mother?
Pt: She died.
Th: So, she died and you didn't give her the affection you wanted to give her in her life?
Pt: Pretty much, yeah. (Tears in his eyes).
Th: Mm‐hmm, how do you feel about that, about not giving her the affection you wanted to give her? (Focus on his guilt about his defense of emotional distancing).
Pt: I feel like a piece of crap. (Tears in his eyes, feeling sadness and guilt about his defenses).
Th: There is a painful feeling in there.
This process above illustrates a small breakthrough of grief and guilt that turned the patient against his own habitual defenses of self‐defeating, emotional detachment and distancing others. Those same distancing behaviors were coming up with the referring therapist manifest a detachment, controlling and competitive behavior to criticize and defeat the therapist. However, at the unconscious level, this patient cannot allow himself to feel this sadness because of the fear of the feelings triggered by caring for himself and being open with another caring person. Now that he has let the therapist in the door, he must, unconsciously, slam it shut and push him out. We continue this interview approximately 5 min later.
Pt: Now I'm fighting with myself because I was a little feeling sorry for myself. But then all my upbringing, all my reserves are going “what do you mean feel sorry for yourself, you don't deserve to feel sorry for yourself.” (Voice of the self‐punishing part of himself).
2.4 | Confronting his defenses: Head‐on collision
The therapist begins a series of interventions confronting the patient with his self‐punitive tendency, his detach- ment and distancing in the office and the impact these actions have on himself and the treatment. Such efforts help turn the patient against his own self‐defeating behavior and at the same time mobilize feelings and memories related to past attachment interruptions.
Th: Something in you says you don't get to feel some sadness for what you wanted and what you also wanted to give but didn't give. You don't get to let yourself feel the guilt about that or the sadness about that. (Emphasizing the self‐defeating part of himself).
Pt: Yeah.
Th: Something says “don't feel that positive feeling. Don't feel that for yourself. You don't deserve to feel good for yourself. You don't deserve to feel that!” (Focusing on the self‐punitive part of himself).
Pt: I don't want to risk feeling that. (The patient is frightened of the self‐punitive part of himself).
Th: But these are ways of not experiencing a feeling right now. Something in you wanted a different re- lationship with your mother, wanted a different relationship with your father, wanted a different relationship with other people, too, but some part of you has held in those feelings and said not to let anyone get close to you anymore. (Emphasizing a drive for love and the impact of his defenses).
Pt: Well I have a friend now that I talk to, but I try not to burden him.
Th: Mm‐hmm. The problem is there's something in there that says put up a wall and keep the feelings all blocked up inside and don't let anyone else get to know those feelings. (Focusing on the defenses related to emotional closeness and the destructive function of defenses).
Pt: Well, in my family that was a weakness. (Insight: a communication that the patient can partially see the past origin of this defense).
Th: Mm‐hmm. For whatever the reason, it's still there; it's part of you that you took in. You bought it. You bought that. (Emphasizing the internal cause of his difficulties).
Pt: Oh, absolutely.
Th: And you said, I'm not letting anyone close to me; I'm keeping all these people away. I'm keeping all the feelings on myself, which is a self‐destructive way of hurting yourself. (Defenses against emotional closeness, self‐ destructiveness).
Pt: Yeah, I see.
Th: But, how do you feel about that because you're a very bright person? We're sitting here talking. That's been something that's been hurting yourself for a long time now and you don't want to live the rest of your life like that, do you? (Emphasizing the self‐defeat, rhetorical question and encouragement to motivate the patient to make changes).
Pt: No.
Th: See there's a painful feeling in there, about this barrier, this wall, but you're holding that back right now here with me. (Encouragement to be present with feelings).
Pt: It probably comes down to self‐image.
Th: It's still a painful feeling right now, though, that you've been holding back. You've been holding this for too long. Haven't you? (Encouragement to be present with feelings).
Pt: Yeah, but I really, honestly, don't know what to do about it. (Insight: the use of negation reveals that he knows what he must do to alter his behavior).
Th: There's a painful feeling in your eyes; there's tears in there that want to come out. You're holding those back though. You fight them off here when we're talking. (Encouragement to feel grief and drop the emotional barrier).
Pt: Oh, absolutely. (Acknowledging the solution is to allow himself to feel).
Th: But if you keep this wall it ends up hurting the opportunity in this minute here with me; doesn't it? (Emphasizing the damage of avoiding his feelings). It hurts the opportunity you have here in this time you have with me; doesn't it? (Highlighting the potential for the partnership). Another hour goes by in your life that you kept things in, you kept people out, and you kept these feelings buried in you. (Emphasizing the nature and impact of defenses). But that's not why you came here, is it? (Encouragement to do good for himself). To keep people out and to bury your feelings?
Pt: No.
Th: So, let's see what we are going to do. As soon as the sadness, the painful feeling and the guilt want to come.... (Encouragement to do his best).
Pt: I shut down. (Sign of patient motivation and insight).
Th: You go detached with me. (Emphasizing the patient is defending against emotional closeness). That means that you hurt what you're trying to do here with me. (Emphasizing the destructive effects). It hurts this opportunity here with me, and it keeps me outside, and I can't be of use to you. (Deactivating the notion of therapist omnipotence).
So, what are we going to do about this, about this barrier here with me, this detachment here with me? (Encouraging a change in behavior). You see it there right now because these feelings want to come, and you put that wall right back up. (Emphasizing the function of the defense).
Pt: Yes.
Th: So, let's see what we can do about this wall. (Encouragement to the therapeutic task and the therapeutic partnership).
2.4.1 | Rupture risk moment
This sequence of statements is intended to highlight the patient's (defenses) pattern of detachment from his feelings and from the therapist and examples of confronting the therapist by devaluing the suggestions being made. This effort motivates him to implement change (via the head‐on collision) and simultaneously triggers positive feelings, anger and guilt about anger related to the therapist efforts. These complex feelings temporarily increase his defenses in the therapeutic relationship. In the previous treatment sessions, his defenses of detachment, controlling, devaluing and arguing became entangled with the therapist resulting in treatment stalemate. The segment that follows is a moment where argument and misalliance could occur as had with the referring therapist: it is a key moment where interventions can help possible self‐defeat turn into a victory for the patient by helping him see and overcome his defenses in the session.
Pt: (Adapts sarcastic and mischievous appearance). Well, you said the magic words. I don't know if it's silly or not, it's when you start using phrases like “here with me”—that strikes me as somewhat formulaic. (Takes a critical position to induce an argument).
Th: Formulaic. But it's you and me here. (Therapist responds, defensively, with a point of debate).
Pt: And the other thing is “how do I feel.” If I knew how I felt, I wouldn't be here. I mean how do I.... (Patient is defending, trying to provoke an argument).
Th: Let me put it another way. Right now, something in you wants to put up some kind of barrier here with me. (Emphasizing the defensive function of the behavior).
Pt: Oh, absolutely! (Smiling and looking relieved the therapist sees the defense).
Th: You had a painful feeling. There's a guilt feeling. There's a craving of closeness that you have within you; these are your emotions that you have. (Clarifying the patient's battle is against part of himself, not between the therapist and him).
Pt: Yes.
Th: At the same time, they want to come, part of you wants to pull back and move away and distance yourself here with me. That's what's happening. I don't know how else to say it, but why do you want to do that to yourself? (Pointing out the complexity of the defense, both the internal nature of his problem and the interpersonal consequences, and attempting to motivate the patient to change). Why do you have a need to put a barrier around yourself, to hurt yourself anymore, to make yourself have to be in a cave, to keep these feelings buried? Why? What crime did you do? This is what I'm saying: “what crime did you do that you have to isolate yourself?” (Highlighting both the self‐punitive and healthy aspects to the patient to motivate change).
Pt: Nothing! (Stated firmly).
Th: So, what are we going to do about this wall and barrier that's coming up here, see because you're still backing away from me? (Encouragement to make change and pointing out ongoing avoidance).
This is a key moment in the process. The patient is repeating his habitual avoidance of potential closeness and feelings relating to closeness through adopting an antagonistic and provocative stance with the therapist. However, at the same time there are signs the patient is now more motivated to make changes and there is a rise in strong feelings with the therapist. The very moment when the therapist could begin an argument with the patient, he instead clarified what was happening: namely that the patient was inadvertently trying to avoid attachment with the therapist. The result is a great deal of relief in the patient, in that the therapist not only was able to see the defense, but also called it out, thereby challenging it in the service of the relationship. This same self‐sabotaging pattern had been going on in all of the patient's prior relationships including his treatment relationships leading to drop‐outs, discord and stalemates for many years.
Pt: That's another coping mechanism. Since meekness didn't work, now I'm going to the attack (Patient de- monstrates insight by referring to his tendency towards devaluation and criticizing, but then suggests his need to create an argument with others).
Th: This is another way to put up a barrier with me.
Pt: Yes!
Th: Okay, so if you don't put a barrier up with me. (Challenging the patient to make changes).
Pt: Well, we're running out of barriers, aren't we? (Marker of increased insight and motivation).
Th: If we do run out then that's good, right? (Therapist and patient both briefly smile).
Pt: Yes, yes, oh absolutely! (Patient is sitting forward in his seat, motivated and engaged).
Th: So here with me you are saying there are many different ways over the years you've kept people at a distance. One way is going on the attack; another is attacking yourself. A bunch of destructive thoughts come. There's the passive waiting. There's isolation. These things have hurt you. How do you feel about that? How do you feel about that when I just said it?
The therapist sensed some sadness emerging in the patient here. This is a self‐compassionate response in the patient for what he has inadvertently done to himself through forming defences that distanced others and harmed himself.
Pt: A little relieved.
Th: Is there some sadness, too, when I said that? (Focus on grief about hurting himself).
Pt: Not yet.
Th: If you're here with me, do you feel that's a sad story? (Focus on grief about hurting himself).
Pt: I've passed over that now. I'm already in my cocoon again.
Th: You felt some sadness again.
Pt: Yeah.
Th: For a second as soon as the sadness came. It's here. It's something we both feel about it, right? As soon as that feeling came... (Emphasizing his feelings and the therapist's own feeling about the patient hurting himself).
Pt: I ran and hid. (A marker of patient insight into his defenses).
Pt: But how do I know I don't deserve it? (A softer position with himself now compared to a few minutes earlier).
Th: So, this is again the barrier that wants to return.
Pt: Oh yeah.
Th: Uh‐huh.
Pt: And feeling sorry for oneself is forbidden. (Therapist understands this as a partial return of patient's self‐punitive tendency).
Th: So that's another barrier.
Pt: That's the barrier. (Insight and motivation to remove the defenses).
Th: Okay, so what are we going to do about that self‐destructive system that wants to operate here with you and me? You and I decided we're going to get to the bottom of this system from where it started and undo it. At the same time, part of you wants to defeat what we're trying to do. Do you follow me? (Emphasizing the task, partnership, barrier and potential for self‐defeat).
Pt: Yeah, but isn't it a pity, and it's destructive as well. (Patient insight and motivation). Th: It's a painful feeling you have.
Pt: It's guilt. (Patient insight).
Th: You've done this even without knowing you've been doing it over the years. You've hurt yourself. You've kept people out. You hurt yourself and didn't even do it on purpose. That's a painful thing. (Encouragement to oppose the defenses).
Pt: How do I know I didn't do it on purpose? (Notice a softer stance toward himself now).
Th: Did you? What crime did you do?
Pt: I wasn't good enough as a person, as a son. No one loved me, so why should I love myself?
Th: What can we do about this remaining barrier here with me. There's a distance still here between us. If you don't go away from me.
A few moments later there is further evidence of the growing shift towards self‐understanding and motivation to change.
Pt: I'm just realizing there's a fear of pushing myself on other people when I'm not wanted. I saw my father do it to my mother all the time. (Insight: link to attachment trauma).
Th: Pushing yourself on people when they don't want it?
Pt: Yeah, a form of mental or emotional rape, I saw my dad do that to my mom.
2.4.2 | Insight and motivation: Unconscious therapeutic alliance
In the following minutes he explained that when his father would abuse his mother, he would provoke his father as a way to stop the abuse. When he provoked the father, the father would attack him and spare the mother.
Pt: I'd still step in when I was a child. Th: Between them, your parents?
Pt: Yeah.
Th: How did you do that?
Pt: You divert his attention by doing something stupid. You start yelling at him, and that would interrupt him.
Th: So, you provoked him to distract him from your mother?
Pt: Yeah. Wow, I hadn't thought of that for a long time. (Marveling at his own insight).
With this information the patient made a direct link between the emotional trauma related to his early attachment relationships and his use of provocation: this same pattern of provoking and arguing was being enacted with the referring therapist. He was then able to feel anger toward his father, guilt about this anger and also grief for his father. Through experiencing some of his feelings about these early family relationships, and subsequent realization that his desire for closeness had become fused with a fear of being harmed, he reduced the likelihood he would need to enact this process again and push away the therapist and others.
Later in the session, a vivid auditory memory arose of his father sexually assaulting his mother when he was under age 5 in a totally dark room they all shared in his apartment at that age: this reflected back to the concept that closeness for him was a “form of mental or emotional rape.”
At the end of the meeting, the patient described his response to the meeting.
Th: Do you think that what we did here today was helpful? When you look at it now? Do you
think that if you get to spend more time on what we did here today, that will free you up in the
future so you don't have to be distant with anybody if you don't want to?
Pt: To answer your question, I've made more progress today than I have in 30 years.
Th: In thirty years?
Pt: Thirty years of trying psychologists and psychiatrists and counselors and, I mean, I started in my twenties asking for help and no one ever got it (understood his self‐defeating defensive tendencies and the underlying trauma).
He went on to summarize his many treatment efforts, including times he had “outsmarted” therapists, laughed at therapists, argued with therapists, and walked out of sessions sensing the treatment could not help him manage his defensive tendencies.
2.4.3 | Outcome and prognosis
Following this trial therapy consultation session, the video of this session was reviewed with the referring therapist. The patient and his therapist had a productive treatment course thereafter, with both of them cognizant of these defensive patterns and where they originated in the patient's childhood. The treating therapist was able to reflect on his own contribution to the interaction problems as well. Together they were able to keep a clear focus on the patient's self‐punitive tendency and use of detachment and avoidance in the treatment sessions; they both avoided engaging in arguments and kept a focus on close collaboration and the feelings and memories this collaboration evoked.
3 | KEY POINTS
Exemplified by the above case, following are some key points to consider when evaluating and treating highly resistant patients who show these common tendencies while expecting and anticipating rupture threats.
4 | CLINICAL PRACTICE AND SUMMARY
Patients who unconsciously erect barriers in relationships due to anxiety about closeness and emotional experi- encing pose a significant challenge for therapists. However, as the therapist attempts to engage the patient, a unique opportunity is formed whereby the patient's most robust habitual ways of avoiding closeness, self‐care and feelings—defenses—can be brought forward, examined, grieved and overcome, giving direct access to the childhood origin of these defensive patterns. These avoidant and self‐defeating behaviours can evoke responses in therapists that make it difficult for the therapist to take a caring position and a help a patient overcome his defenses. However, persisting to do one's best for the patient while helping the patient turn against these defenses, can bring a marked change in the process from both the therapist and patient perspective. We believe that this is one way to conceptualize rupture moments in psychotherapy and, in doing so, improve the likelihood of a positive therapeutic experience.
Correspondence
Allan A. Abbass, 7518‐5909 Veterans Memorial Ln, Halifax, NS B3H 2E2, Canada.
Email: allan.abbass@dal.ca
DATA AVAILABILITY STATEMENT
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
ORCID
Allan A. Abbass https://orcid.org/0000-0003-1285-5770
REFERENCES
Abbass, A. (2015). Reaching through resistance: Advanced psychotherapy techniques. Seven Leaves Press.
Abbass, A. (2016). The Emergence of psychodynamic psychotherapy for treatment resistant patients: Intensive short‐term dynamic psychotherapy. Psychodynamic Psychiatry, 44(2), 245–280. https://doi.org/10.1521/pdps.2016.44.2.245
Abbass, A., & Katzman, J. (2013). The cost‐effectiveness of intensive short‐term dynamic psychotherapy. Psychiatric Annals,43, 496–501. 10.3928/00485713‐20131105‐04
Abbass, A., Kisely, S., & Kroenke, K. (2009). Short‐term psychodynamic psychotherapy for somatic disorders, Systematic review and meta‐analysis of clinical trials. Psychotherapy and Psychosomatics, 78(5), 265–274.
Abbass, A., Town, J., & Driessen, E. (2012). Intensive short‐term dynamic psychotherapy: A systematic review and meta‐ analysis of outcome research. Harvard Review of Psychiatry, 20(2), 97–108. https://doi.org/10.3109/10673229.2012.677347
Abbass, A. A., & Town, J. M. (2013). Key clinical processes in intensive short‐term dynamic psychotherapy. Psychotherapy (Chic), 50(3), 433–437. https://doi.org/10.1037/a0032166
Bowlby, R. J. M., & Gatling, A. (1988). A secure base: Parent‐child attachment and healthy human development. Routledge.
Crits‐Christoph, P., Cooper, A., & Luborsky, L. (2003). The measurement of accuracy of interpretations. In L. Luborsky, & P. Crits‐Christoph (Eds.), Understanding transference: The CCRT method (2nd ed., pp. 197–212). American Psychological Association.
Crits‐Christoph, P., Cooper, A., & Luborsky, L. (1988). The accuracy of therapists' interpretations and the outcome of dynamic psychotherapy. Journal of Consulting and Clinical Psychology, 56, 490–495.
Davanloo, H. (1990). Unlocking the unconscious: Selected papers of Habib Davanloo. John Wiley & Sons.
Davanloo, H. (2000). Intensive short‐term dynamic psychotherapy: Selected papers of Habib Davanloo. Wiley.
Davanloo, H. (2001). Intensive short‐term dynamic psychotherapy: Extended major direct access to the unconscious.
European Psychotherapy, 2(1), 25–70.
Eubanks, C. F., Muran, J. C., & Safran, J. D. (2015). Rupture resolution rating system (3RS): Manual. Mount Sinai Beth Israel
Medical Center.
Eubanks, C. F., Muran, J. C., & Safran, J. D. (2018). Alliance rupture repair: A meta‐analysis. Psychotherapy, 55, 508–519.https://doi.org/10.1037/pst0000185
Gerostathos, A., de Roten, Y., Berney, S., Despland, J. N., & Ambresin, G. (2014). How does addressing patient's defenses help to repair alliance ruptures in psychodynamic psychotherapy?: An exploratory study. The Journal of Nervous and Mental Disease, 202(5), 419–424.
Granqvist, P., Sroufe, L. A., Dozier, M., Hesse, E., Steele, M., van Ijzendoorn, M., Solomon, J., Schuengel, C., Fearon, P., Bakermans‐ Kranenburg, M., Steele, H., Cassidy, J., Carlson, E., Madigan, S., Jacobvitz, D., Foster, S., Behrens, K., Rifkin‐Graboi, A., Gribneau, N., ... Duschinsky, R. (2017). Disorganized attachment in infancy: A review of the phenomenon and its implications for clinicians and policy‐makers. Attachment & Human Development, 19(6), 534–558.
Kramer, U., Pascual‐Leone, A., Despland, J. N., & De Roten, Y. (2014). Emotion in an alliance rupture and resolution sequence: A theory‐building case study. Counselling and Psychotherapy Research, 14(4), 263–271.
Michel, L., Kramer, U., & De Roten, Y. (2011). Alliance evolutions over the course of short‐ term dynamic psychotherapy: A case study. Counselling and Psychotherapy Research, 11(1), 43–54.
Safran, J. D., & Muran, J. C. (2000). Negotiating the therapeutic alliance: a relational treatment guide. Guilford Press.
Sahli, C., de Roten, Y., & Despland, J. N. (2015). Therapist interpretation, alliance rupture—resolution and outcome. Swiss Archives of Neurology and Psychiatry, 166(6), 208–221.
Town, J. M., Abbass, A., & Bernier, D. (2013). Effectiveness and cost effectiveness of Davanloo's intensive short‐term dynamic psychotherapy: Does unlocking the unconscious make a difference? American Journal of Psychotherapy, 67(1),89–108.
Town, J., Salvadori, A., Falkenström, F., Bradley, S., & Hardy, G. (2017). Is affect experiencing therapeutic in major depressive disorder? Examining associations between affect experiencing and changes to the alliance and outcome in intensive short‐term dynamic psychotherapy. Psychotherapy, 54(2), 148–158.
Town, J. M., Hardy, G. E., McCullough, L., & Stride, C. (2012). Patient affect experiencing following therapist interventions in short‐term dynamic psychotherapy. Psychotherapy Research, 22(2), 208–219. https://doi.org/10.1080/10503307.2011. 637243
How to cite this article: Abbass AA, Town JM. Alliance rupture‐repair processes in intensive short‐term dynamic psychotherapy: Working with resistance. J. Clin. Psychol. 2021;77:398–413. https://doi.org/10.1002/jclp.23115
/*Aenderungen verstecken*/
Neuen Kommentar hinzufügen